Medication Management After Weight Loss Surgery
Guide to Medication Management after Bariatric Surgery
Two years after my weight loss surgery (gastric bypass), I discovered something my pre-surgical education hadn’t fully prepared me for: my medications worked completely differently. The antidepressants that had kept me stable for years suddenly caused side effects, and my blood pressure medication seemed far too potent. I quickly learned that proper medication management after weight loss surgery isn’t just helpful, it’s essential for your health and recovery.
If you’re considering or have recently undergone bariatric surgery, understanding how your body now processes medications could be critical for your ongoing well-being. In this post i’ll share what I’ve learned about managing medications after my surgery and why proper dosage adjustments matter more than you might realize.
Understanding How Weight Loss Surgery Alters Medication Absorption
Different types of surgery affect absorption in various ways. The anatomical changes caused by these procedures fundamentally alter how your body processes what you ingest, often requiring adjustments to medication regimens. After my bypass, I experienced firsthand how these changes can impact daily medication management. Alterations to my digestive tract meant medications were absorbed differently, sometimes unpredictably.
The Science Behind Altered Absorption
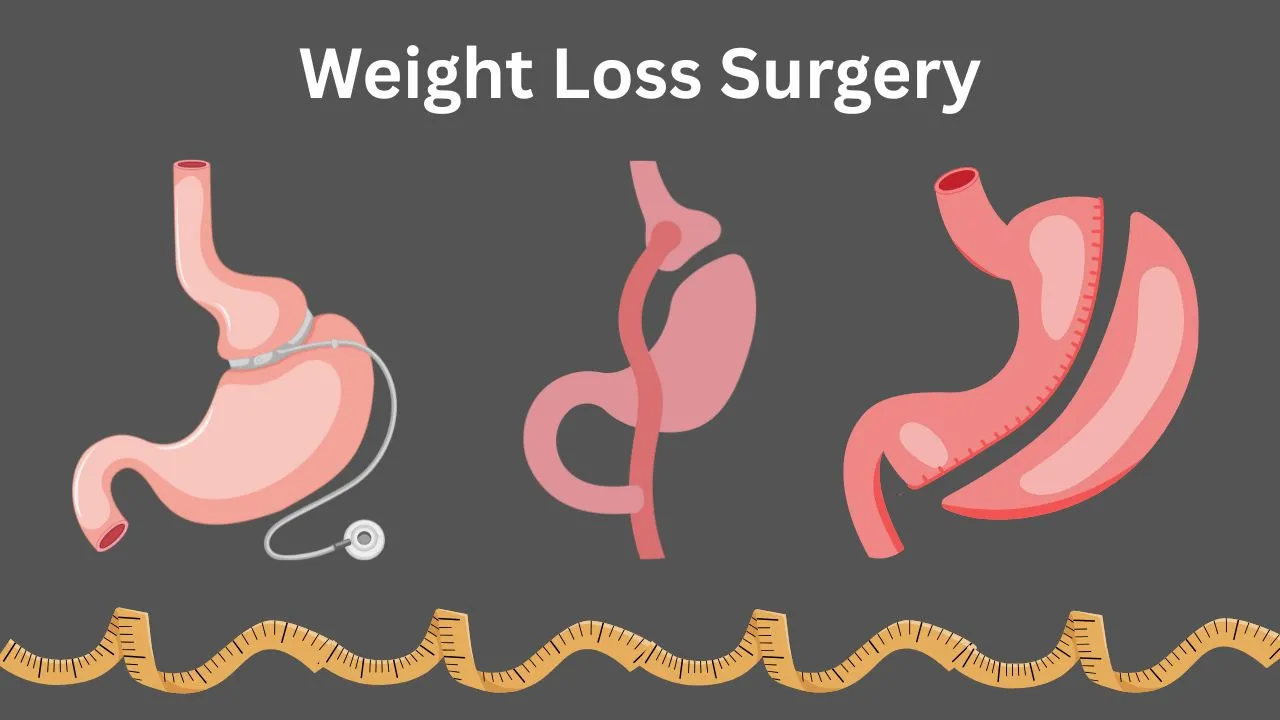
With procedures like gastric bypass, duodenal switch, and even sleeve gastrectomy, your stomach size is dramatically reduced, and portions of your small intestine are bypassed. Since the small intestine is the primary site for medication absorption, these changes can create several significant effects:
Immediate-release: Your doctor might switch you to regular, immediate-release (IR) versions, which may need to be taken in smaller amounts more frequently. For the first few months, you may also need to use liquid formulations or crush tablets. These changes can lead to medications being either under-absorbed (making them less effective) or over-absorbed (potentially causing toxicity). I experienced both scenarios with different medications after my surgery.
How Does Each Procedure Affect Medications?
Each type of weight loss surgery affects absorption differently. Understanding which procedure you have undergone is essential for proper medication management.
Roux-en-Y Gastric Bypass
The Roux-en-Y procedure, which I underwent, creates a small stomach pouch (about the size of an egg) and bypasses a significant portion of the small intestine. This surgery significantly affects medication absorption because it:
Sleeve Gastrectomy (Gastric Sleeve)
Also called Gastric Sleeve, this procedure removes approximately 80% of the stomach but leaves the intestinal tract intact. Its effects on medication absorption include:
While it generally has less impact on absorption than bypass procedures, monitoring is still important.
Duodenal Switch
The Duodenal Switch is a complex procedure with significant effects on medication absorption. It combines a sleeve gastrectomy with a long intestinal bypass, which:
Adjustable Gastric Band (Lap-Band)
The Adjustable Gastric Band involves placing an inflatable band around the upper part of the stomach. Unlike other procedures, it has minimal impact on medication absorption because it does not alter the anatomy of the stomach or intestines. However, it can affect how quickly large pills pass into the stomach.
Which Medications Often Require Adjustment After weight loss surgery?
Based on my experience and extensive research, the following types of medications often need the most attention after bariatric surgery.
Blood Pressure and Heart Medications
These medications frequently require significant dosage reductions after bariatric surgery. My own experience with my blood pressure medication becoming too potent is a well-documented clinical outcome.
A landmark study known as the GATEWAY trial found that five years after Roux-en-Y gastric bypass, 46.3% of patients achieved complete hypertension remission, meaning they no longer needed any medication to control their blood pressure. This was compared to just 2.4% of patients treated with medication alone. The study also showed that 83.7% of surgical patients (41 out of 49 in the gastric bypass group) were able to reduce their antihypertensive medications by at least 30% while maintaining controlled blood pressure at 12 months.
Diabetes Medications
Many patients experience immediate improvements in insulin sensitivity after weight loss surgery, often before significant weight loss occurs . This frequently requires rapid adjustments to diabetes medications. A large Australian study found that among patients treated for diabetes before surgery, 71.6% required no diabetes medication at all just 12 months later. Even five years post-surgery, 61% remained off all diabetes medications .
Pain Medications and Anti-inflammatories (NSAIDs)
This is a critically important area. A vital safety rule after bariatric surgery involves non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Advil, Motrin) and naproxen (Aleve).
Mental Health Medications
Antidepressants and other psychiatric medications can be significantly affected. As you lose weight, the distribution of fat-soluble (lipophilic) drugs in your body changes, and altered absorption can lead to unpredictable blood levels. It’s really important to work closely with your mental health provider, as regular monitoring and dosage adjustments may be needed. The journey can be emotionally challenging, and finding a supportive community can be incredibly helpful for navigating these changes.
Thyroid Medications
Thyroid medication absorption, particularly levothyroxine, can be significantly reduced after bypass procedures. A common and critical mistake is taking thyroid medication at the same time as certain supplements. To ensure your medication works correctly, it is usually recommended to take it at least 1 to 2 hours apart from any supplements containing calcium or iron.
Oral Contraceptives
A vital piece of safety information that is often overlooked is the impact of bariatric surgery on the effectiveness of oral contraceptives (birth control pills). Due to changes in absorption, pills may not be reliably absorbed after surgery, significantly increasing the risk of unintended pregnancy. It is strongly recommended to discuss more reliable, non-oral birth control methods with your gynecologist, such as an IUD, implant, patch, or shot.
How to Effectively Communicate With Your Healthcare Team
Proactive communication with all my healthcare providers about my bypass was the most important lesson I learned.
Effective Communication Tips:
Taking Control of Your Health Journey
Ten years after my surgery, I’ve learned that successful medication management requires vigilance, education, and partnership with healthcare providers. The changes to how my body processes medications weren’t something I fully anticipated before my gastric bypass, but with proper adjustments, my medications now work effectively.
If you have had or are thinking about weight loss surgery, it’s important to check all your medications. The surgery can help with many health issues but may also affect how your body absorbs medicines, so your treatments might need to change.
References
The GATEWAY Randomized Trial (Gastric Bypass to Treat Obese Patients With Steady Hypertension). PubMed
TCTMD. (2024, February 5). BP Reductions Last 5 Years After Bariatric Surgery: GATEWAY. Link
Journal of the American College of Cardiology. (2024). Five-Year Outcomes of Gastric Bypass vs Medical Therapy for Obese Patients With hypertension. Link
American College of Cardiology. (2024, February 5). Study: Weight-Loss Surgery Most Effective for Long-term Blood Pressure Control. Link
Kaiser Permanente. (n.d.). Safe Medication Use After Weight Loss Surgery. Link
British Obesity & Metabolic Surgery Society (BOMSS). (n.d.). BOMSS Guidance on Medications Post-Bariatric Surgery for GPs. Link
Segal, J.B., et al. (2017). Bariatric Surgery: Impact on Medication Management. ResearchGate
Papamargaritis, D., et al. (2020). The Effects of Bariatric Surgery on the Pharmacokinetics of Drugs: A Review of Current Evidence. PMC Article
Crasset, C., et al. (2020). Medication Management in Patients Who Have Had Bariatric Surgery. PMC Article
UCSF Health. (n.d.). Life After Bariatric Surgery. Link
Specialist Pharmacy Service – NHS. (n.d.). Considerations for Using Medicines Following Bariatric Surgery. Link
Kaiser Permanente. (n.d.). Weight Loss Surgery Procedures: Gastric Sleeve and Gastric Bypass. Link
Monash University. (2025, February 12). Bariatric Surgery Is Safe and Reduces the Need for Diabetes Medication: Study. Link
Taylor Bariatric. (n.d.). Which Medications Should You Avoid After Bariatric Surgery? Link
Kaiser Permanente. (n.d.). Weight Loss Surgery, Birth Control, and Pregnancy. Link
Kaiser Permanente. (n.d.). Top 10 Factors to Consider Before Choosing Weight Loss Surgery. Link
Kaiser Permanente. (n.d.). Weight Loss Surgery. Link